We diagnose and treat many conditions of the bowel and colon including colitis, rectal prolapse, constipation and many more. Read more about some of these conditions or contact us to ask a question or make an an appointment.
Ulcerative Colitis
What is ulcerative colitis?
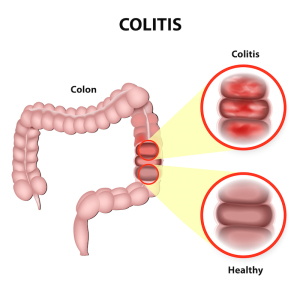
Ulcerative colitis is an inflammation of the lining of the large bowel (colon). Symptoms include rectal bleeding, diarrhea, abdominal cramps, weight loss, and fevers. In addition, patients who have had extensive ulcerative colitis for many years are at an increased risk to develop large bowel cancer. The cause of ulcerative colitis remains unknown.
How is ulcerative colitis treated?
Initial treatment of ulcerative colitis is medical, using antibiotics and anti-inflammatory medications such as Alzulfidine or Prednisone. These are usually necessary on a long-term basis. Prednisone has significant side effects, and, therefore, it is usually used for short periods. Flare-ups of the disease can often be treated by increasing the dosage of medications or adding new medications, such as 6-Mercaptopurine. Hospitalization may be necessary to put the bowel to rest.
When is surgery necessary?
Surgery is indicated for patients who have life-threatening complications of inflammatory bowel diseases, such as massive bleeding, perforation, or infection. It may also be necessary for those who have the chronic form of the disease, which fails medical therapy. It is important the patient be comfortable that all reasonable medical therapy has been attempted prior to considering surgical therapy. In addition, patients who have long-standing ulcerative colitis and show cancer signs may be candidates for removal of the colon, because of the increased risk of developing cancer. More often, these patients are followed carefully with repeated colonoscopy and biopsy, and only if precancerous signs are identified is surgery recommended.
What operations are available?
Historically, the standard operation for ulcerative colitis has been removal of the entire colon, rectum, and anus. This operation is called a proctocolectomy and may be performed in one or more stages. It cures the disease and removes all risk of developing cancer in the colon or rectum.
However, this operation requires creation of a Brooke ileostomy and chronic use of an appliance on the abdominal wall to collect waste from the bowel.
The continent ileostomy is similar to a Brooke ileostomy, but an internal reservoir is created. The bowel still comes through the abdominal wall, but an external appliance is not required. The internal reservoir is drained three to four times a day by inserting a tube into the reservoir. This option eliminates the risks of cancer and risks of recurrent persistent colitis, but the internal reservoir may begin to leak and require another surgical procedure to revise the reservoir.
Some patients may be treated by removal of the colon, with preservation of the rectum and anus. The small bowel can then be reconnected to the rectum and continence preserved. This avoids an ileostomy, but the risks of ongoing active colitis, increased stool frequency, urgency, and cancer in the retained rectum remain.
Are there other surgical alternatives?
The ileoanal procedure is the newest alternative for the management of ulcerative colitis. This procedure removes all of the colon and rectum, but preserves the anal canal. The rectum is replaced with small bowel, which is refashioned to form a small pouch. Usually, a temporary ileostomy is created, but this is closed in several months. The pouch acts as a reservoir to help decrease the stool frequency. This maintains a normal route of defecation, but most patients experience five to ten bowel movements per day. This operation all but eliminates the risk of recurrent ulcerative colitis and allows the patient to have a normal route of evacuation. Patients can develop inflammation of the pouch, which requires antibiotic treatment. In a small percentage of patients, the pouch fails to function properly and may have to be removed. If the pouch is removed, a permanent ileostomy will likely be necessary.
Which alternative is preferred?
It is important to recognize that none of these alternatives makes a patient with ulcerative colitis normal. Each alternative has perceivable advantages and disadvantages, which must be carefully understood by the patient prior to selecting the alternative which will allow the patient to pursue the highest quality of life.
Rectal Prolapse
What is rectal prolapse?
Rectal prolapse is a condition in which the rectum, the lower end of the colon, located just above the anus, turns itself inside out. In the earliest phases of this condition, the rectum does not stick out of the body, but as the condition worsens, it may protrude. Weakness of the anal sphincter muscle is often associated with rectal prolapse at this stage and may result in leakage of stool or mucus. The condition occurs in both sexes, although it is more common in women than men.
Why does it occur?
Several factors may contribute to the development of rectal prolapse. It may come from a lifelong habit of straining to have bowel movements or as a delayed result of stresses involved in childbirth. In rare cases, there may be a genetic predisposition in some families. It seems to be a part of the aging process in many patients who experience weakening of the ligaments that support the rectum inside the pelvis as well as loss of tightness of the anal sphincter muscle. In some cases, neurological problems, such as spinal cord transection or spinal cord disease, can lead to prolapse. In most cases, however, no single cause can be identified.
Is rectal prolapse the same as hemorrhoids?
Some of the symptoms may be the same. There may be bleeding and/or tissue that protrudes from the rectum. Rectal prolapse, however, involves a segment of the bowel located higher up within the body, while hemorrhoids develop near the anal opening.
How is rectal prolapse diagnosed?
Our physicians can diagnose this condition by taking a careful history and performing a complete anorectal examination. To demonstrate the prolapse, patients may be asked to “strain” as if having a bowel movement or to sit on the commode and “strain” prior to examination.
At times, however, a rectal prolapse may be hidden or internal. In this situation, an x-ray examination called a videodefecogram may be helpful. This examination, which takes x-ray pictures while the patient is having a bowel movement, can also assist the physician in determining whether surgery may be beneficial and which operation may be appropriate.
Anorectal manometry may also be used. This test measures whether or not the muscles around the rectum are functioning normally.
How is rectal prolapse treated?
Although constipation and straining may be causes of rectal prolapse, simply correcting these problems may not improve the prolapse once it has developed. There are many different ways to surgically correct rectal prolapse.
Abdominal or rectal surgery may be suggested. Your doctor can help you decide which method will most likely achieve the best result by taking into account many factors, such as age, physical condition, extent of prolapse and the results of various tests.
Treatment of Rectal Prolapse depends on several factors:
- Patient’s age
- Physical condition
- Extent of prolapse
- Test results
How successful is treatment?
Success depends on a number of factors, including the status of a patient’s anal sphincter muscle before surgery, whether the prolapse is internal or external, the overall condition of the patient and surgical method used. If the anal muscle has been weakened, either because of the rectal prolapse or for some other reason, it may in many cases significantly regain strength after the rectal prolapse has been corrected.
Chronic constipation and straining after surgical correction must be avoided. A great majority of patients are completely relieved of symptoms, or are significantly helped, by the appropriate procedure.
Constipation
What is constipation?
Constipation uncomfortable and has different meanings to different individuals.
Most commonly, it refers to infrequent bowel movements, but may also refer to a decrease in the volume or weight of stool, the need to strain to have a movement, a sense of incomplete evacuation, or the need for enemas, suppositories or laxatives to maintain regularity.
For most people, it is normal for bowel movements to occur from three times a day to three times a week. Other people may go a week or more without experiencing discomfort or harmful effects. About 80 percent of people suffer from constipation at some time during their lives, and brief periods of constipation are normal.
Normal bowel habits are affected by diet. The average American diet includes 12 to 15 grams of fiber per day, although for proper bowel function 25 to 30 grams of fiber and about 60 to 80 ounces of fluid are recommended each day. Exercise is also beneficial to proper function of the colon.

Eating foods high in fiber, including bran, shredded wheat, whole grain breads and certain fruits and vegetables will help provide the 25 to 30 grams of fiber per day recommended for proper bowel function.
How is constipation diagnosed?
Constipation may be diagnosed if bowel movements occur fewer than three times weekly on an ongoing basis. Widespread beliefs, such as the assumption that everyone should have a movement at least once each day, have led to overuse and abuse of laxatives.
What causes constipation?
There may be several, possibly simultaneous, causes for constipation, including inadequate fiber and fluid intake, a sedentary lifestyle, and environmental changes. Constipation may be aggravated by travel, pregnancy or change in diet. In some people, it may result from repeatedly ignoring the urge to have a bowel movement.
More serious causes of constipation include growths or areas of narrowing in the colon, so it is wise to seek the advice of a colon and rectal surgeon when constipation persists. Constipation may rarely be a symptom of scieroderma, lupus, or disorders of the nervous or endocrine systems, including thyroid disease, multiple sclerosis, Parkinson’s disease, stroke, and spinal cord injuries.
Can medication cause constipation?
Yes, many medications, including pain killers, antidepressants, tranquilizers, and other chiatric medications, blood pressure medication, diuretics, iron supplements, calcium supplements, and aluminum containing antacids can cause or worsen constipation.
Some people who are not actually constipated may become dependent on laxatives in an ill advised attempt to have daily bowel movements, and many cause themselves harm through laxative abuse.
When should I see a doctor about constipation?
Any persistent change in bowel habit – increase or decrease in frequency or size of stool or an increased difficulty in evacuating – warrants medical advice. Whenever constipation symptoms persist for more than three weeks, you should consult your physician. If blood appears in the stool, consult your colon and rectal surgeon right away.
How can the cause of constipation be determined?
Constipation may have many causes, and it is important to identify them so that treatment can be as simple and specific as possible. Your doctor will want to check for any anatomic causes, such as growths or areas of narrowing in the colon.
Digital examination of the anorectal area is usually the first step, since it is relatively simple and may provide clues to the underlying causes of the problem. Examination of the intestine with either a flexible lighted instrument or barium x-ray study may help pinpoint the problem and exclude serious conditions known to cause constipation, such as polyps, tumors, or diverticular disease. If an anatomic problem is identified, treatment can be directed toward correcting the abnormality.
Other tests may identify specific functional causes to help direct treatment. For example, “marker studies,” in which the patient swallows a capsule containing markers that show up on x-rays taken repeatedly over several days, may provide clues to disorders in muscle function within the intestine. Other physiologic tests evaluate the function of the anus and rectum. These tests may involve evaluating the reflexes of anal muscles that control bowel movements using a small plastic catheter, or x-ray testing to evaluate function of the anus and rectum during defecation.
In many cases, no specific anatomic or functional causes are identified and the cause of constipation is said to be nonspecific.
How is constipation treated?
The vast majority of patients with constipation are successfully treated by adding high fiber foods like bran, shredded wheat, whole grain breads and certain fruits and vegetables to the diet, along with increased fluids. Your physician may also recommend lifestyle changes. Fiber supplements containing undigestible vegetable fiber, such as bran, are often recommended and may provide many benefits in addition to relief of constipation. They may help to lower cholesterol levels, reduce the risk of developing colon polyps and cancer, and help prevent symptomatic hemorrhoids.
Fiber supplements may take several weeks, possibly months, to reach full effectiveness, but they are neither harmful nor habit forming, as some stimulant laxatives may become with overuse or abuse. Other types of laxatives, enemas or suppositories should be used only when recommended and monitored by your colon and rectal surgeon.
Designating a specific time each day to have a bowel movement also may be very helpful to some patients. In some cases, bio-feedback may help to retrain poorly functioning anal sphincter muscles. Only in rare circumstances are surgical procedures necessary to treat constipation. Your colon and rectal surgeon can discuss these options with you in greater detail to determine the best treatment for you.